The macula or macula lutea (from Latin macula, “spot” + lutea, “yellow”) is an oval-shaped highly pigmented yellow spot near the center of the retina of the human eye. It has a diameter of around 6 mm and is often histologically defined as having two or more layers of ganglion cells. Near its center is the fovea, a small pit that contains the largest concentration of cone cells in the eye and is responsible for central, high resolution vision. The macula also contains the parafovea and perifovea.
Because the macula is yellow in color it absorbs excess blue and ultraviolet light that enter the eye, and acts as a natural sunblock (analogous to sunglasses) for this area of the retina. The yellow colour comes from its content of lutein and zeaxanthin, which are yellow xanthophyll carotenoids, derived from the diet. Zeaxanthin predominates at the macula, while lutein predominates elsewhere in the retina. There is some evidence that these carotenoids protect the pigmented region from some types of macular degeneration.
Structures in the macula are specialized for high acuity vision. Within the macula are the fovea and foveola which contain a high density of cones (photoreceptors with high acuity).
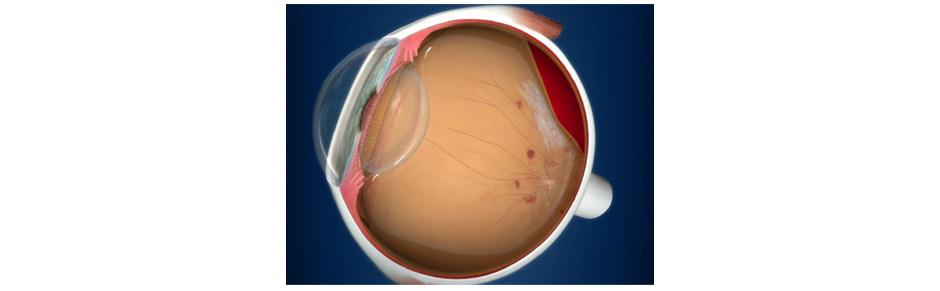
Age-related macular degeneration (AMD) is a medical condition which usually affects older adults and results in a loss of vision in the center of the visual field (the macula) because of damage to the retina. It occurs in “dry” and “wet” forms. It is a major cause of blindness and visual impairment in older adults (>50 years). Macular degeneration can make it difficult or impossible to read or recognize faces, although enough peripheral vision remains to allow other activities of daily life.
Starting from the inside of the eye and going towards the outer surface, the three main layers at the back of the eye are the retina, which is light-sensitive tissue that is considered part of the central nervous system and is actually brain tissue; the choroid, which contains the blood supply; and the sclera, which is the white, outer, layer of the eye.
The macula is the central area of the retina, which provides the most detailed central vision.
In the dry (nonexudative) form, cellular debris called drusen accumulates between the retina and the choroid, and the retina can become detached. In the wet (exudative) form, which is more severe, blood vessels grow up from the choroid behind the retina, and the retina can also become detached. It can be treated with laser coagulation, and with medication that stops and sometimes reverses the growth of blood vessels.
Although some macular dystrophies affecting younger individuals are sometimes referred to as macular degeneration, the term generally refers to age-related macular degeneration (AMD or ARMD).
Age-related macular degeneration begins with characteristic yellow deposits (drusen) in the macula, between the retinal pigment epithelium and the underlying choroid. Most people with these early changes (referred to as age-related maculopathy) have good vision. People with drusen can go on to develop advanced AMD. The risk is higher when the drusen are large and numerous and associated with disturbance in the pigmented cell layer under the macula. Large and soft drusen are related to elevated cholesterol deposits and may respond to cholesterol-lowering agents.
Signs and symptoms of macular degeneration include:
- Drusen
- Pigmentary alterations
- Exudative changes: hemorrhages in the eye, hard exudates, subretinal/sub-RPE/intraretinal fluid
- Atrophy: incipient and geographic
- Visual acuity drastically decreasing (two levels or more), e.g.: 20/20 to 20/80.
- Preferential hyperacuity perimetry changes (for wet AMD)
- Blurred vision: Those with nonexudative macular degeneration may be asymptomatic or notice a gradual loss of central vision, whereas those with exudative macular degeneration often notice a rapid onset of vision loss. This is often caused by age.
- Central scotomas (shadows or missing areas of vision)
- Distorted vision in the form of metamorphopsia, in which a grid of straight lines appears wavy and parts of the grid may appear blank: Patients often first notice this when looking at miniblinds in their home.
- Trouble discerning colors, specifically dark ones from dark ones and light ones from light ones
- Slow recovery of visual function after exposure to bright light
- A loss in contrast sensitivity
- Macular degeneration by itself will not lead to total blindness. For that matter, only a very small number of people with visual impairment are totally blind. In almost all cases, some vision remains. Other complicating conditions may possibly lead to such an acute condition (severe stroke or trauma, untreated glaucoma, etc.), but few macular degeneration patients experience total visual loss.The area of the macula comprises only about 2.1% of the retina, and the remaining 97.9% (the peripheral field) remains unaffected by the disease. Interestingly, even though the macula provides such a small fraction of the visual field, almost half of the visual cortex is devoted to processing macular information.
- The loss of central vision profoundly affects visual functioning. It is quite difficult, for example, to read without central vision. Pictures that attempt to depict the central visual loss of macular degeneration with a black spot do not really do justice to the devastating nature of the visual loss. This can be demonstrated by printing letters six inches high on a piece of paper and attempting to identify them while looking straight ahead and holding the paper slightly to the side. Most people find this difficult to do.
- There is a loss of contrast sensitivity, so that contours, shadows, and color vision are less vivid. The loss in contrast sensitivity can be quickly and easily measured by a contrast sensitivity test performed either at home or by an eye specialist.
- Similar symptoms with a very different etiology and different treatment can be caused by epiretinal membrane or macular pucker or leaking blood vessels in the eye.